Digital therapeutics informed by lived experience.
Living well beyond chronic illness.
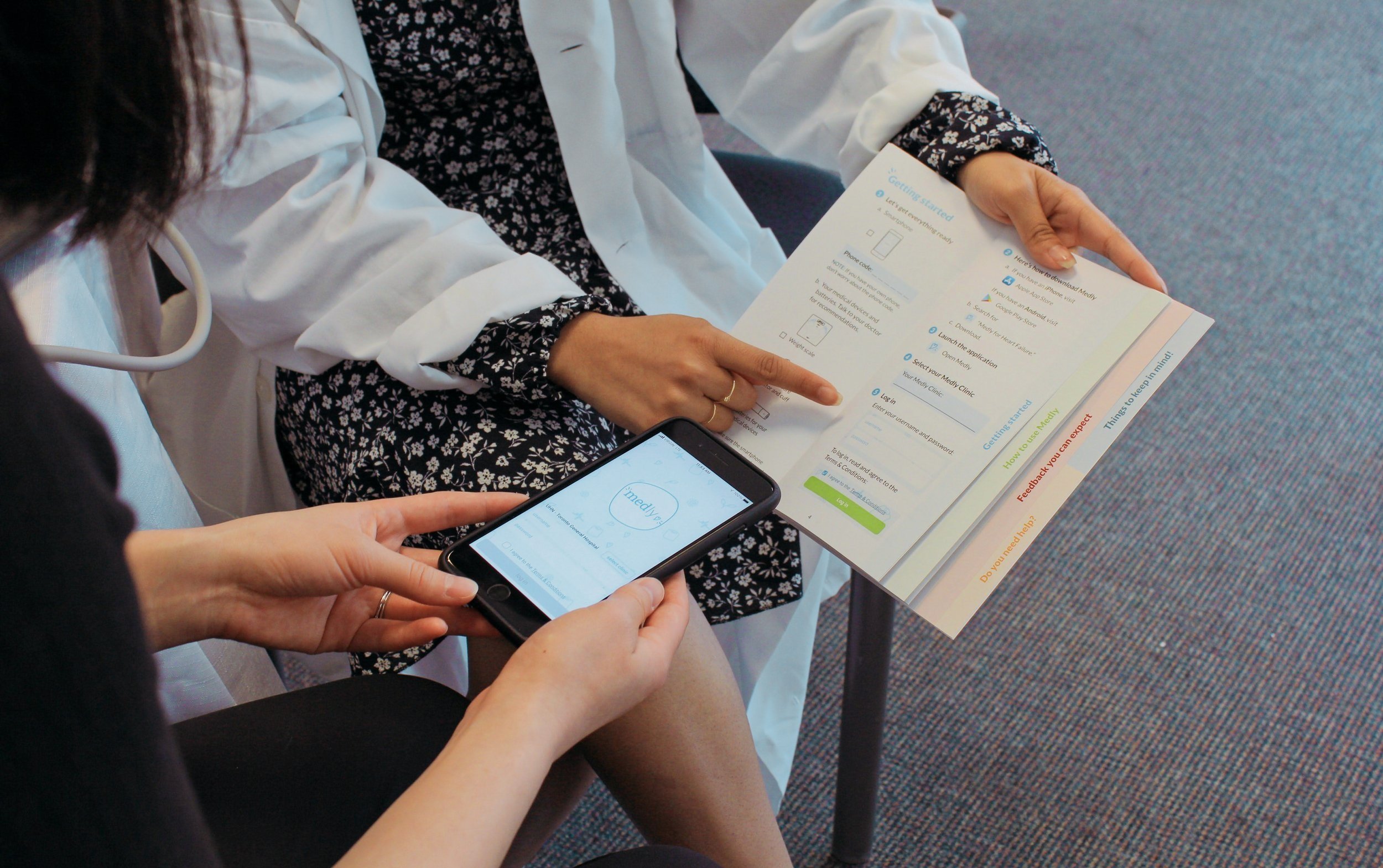
Digital therapeutics are transforming traditional healthcare delivery. Our solutions aim to engage and empower patients through the use of technology to become partners in their own healthcare.
Tackling some of healthcare’s biggest challenges from within the system.
Based inside the Toronto General Hospital
We collaborate with our patient partners and clinician champions to understand the lived experience of chronic illness and address therapeutic gaps.
What matters to us.
-

Pushing boundaries in care
-

Building effective expert systems
-

Implementing within diverse environments
-

Creating measurable and meaningful value
Find out more about what we’re up to at the Centre.
Notable publications.
Bridging technological advancements with clinical insights, we contribute to the research community through our high-quality, peer-reviewed publications.
-

Outcomes of a Heart Failure Telemonitoring Program Implemented as the Standard of Care in an Outpatient Heart Function Clinic: Pretest-Posttest Pragmatic Study. Read More
-

A Patient-Centered Mobile Health System That Supports Asthma Self-Management (breathe): Design, Development, and Utilization. Read More
-

Design of an mHealth app for the self-management of adolescent type 1 diabetes: a pilot study. Read More
-
Mobile Phone-Based Telemonitoring for Heart Failure Management: A Randomized Controlled Trial. Read More






